Stijn Plessers holds a degree in Economics (Catholic University of Leuven). He started his career in 2006 at a private bank and then worked for KBC Asset Management for 15 years. At KBC AM, he was originally responsible for managing a large credit and OTC derivatives portfolio before focusing entirely on equities. First as an analyst for the technology sector and then as a manager of specialized, global equity mandates. In April 2023, Stijn made the switch to Econopolis Wealth Management.
Obesity: A Price Tag on Pounds and Pills – Finding the Balance

Obesity: What Are We Solving For?
The discourse surrounding the optimal treatment for obesity - and its corresponding financial reimbursements – is currently in the spotlight. This renewed interest is spurred by the rapid emergence of a new class of injectable weight-loss treatments: the GLP1 drugs. GLP-1 or glucagon-like peptide-1, is a hormone released in the gut after food intake. It plays multiple roles in maintaining blood sugar balance.
For years, the pharmaceutical market has witnessed a series of drugs that either delivered mediocre results in weight loss or brought with them a slew of serious side effects. However, a turning point appeared with the introduction of semaglutide, a synthetic version of GLP-1. Initially conceptualized as a remedy for diabetes, this compound underwent clinical trials by the Danish firm Novo Nordisk on obese patients who weren’t diabetic. The findings, disseminated in 2021, were promising: individuals administered with the weekly injection lost an average of nearly 15% of their total body weight. In contrast, those who relied solely on diet and exercise experienced a weight loss of just about 2%.
A Chronic Disease or A Choice?
Despite influential organizations like the American Medical Association – considered the most influential medical association in the US – declaring obesity a disease over a decade ago, the debate has never really settled. If we were to work with a universally accepted definition of 'disease' ((a topic worthy of its own discussion), then classifying obesity as such would suggest that tens of millions of people must now have bodies or minds, or both, that are not working properly. This classification would mean that that even those who appear healthy but are overweight — encompassing both adults and children alike — are, by this definition, afflicted with a disease.
On the other hand, twin and adoption studies show the significant role of genetics in BMI variations. It’s estimated that genetics could account for up to 70% of the variation in obesity, impacting energy intake, expenditure, and the regulation of satiety signals. While rare genetic defects like leptin deficiency have been linked to obesity, more prevalent gene variations seem to have a more subtle impact on weight. No single, widespread gene has been identified that can explain obesity. Instead, it seems a combination of genes are involved in the heritability and susceptibility for obesity.
This discussion obviously ties into the debate on the appropriate treatment for obesity. Labelling it has profound implications for society and requires careful reflection. The categorization of obesity as a disease has a pernicious influence on efforts to remedy the problem at its true origins. The treatment of diseases customarily involves drugs, medical technology, clinic visits and surgical procedures. If obesity is a disease, the therapeutic advances on which its management depends presumably reside in these domains. However, before delving into potential treatments, it's crucial to grasp the sheer scale of the issue.
Western Epidemic or Pandemic?
Regardless of its classification as a disease, there's no denying the enormity of the challenge posed by obesity. This is underscored by the recent findings presented in the 'World Obesity Atlas 2023' by the World Obesity Federation, an NGO recognized by the World Health Organization (WHO). According to the study, today around 1.1 billion people aged five and older, which equates to around 14% of the global population in that age bracket, are obese. On top of that a further 1.6 billion people, or 24% of the world’s population aged five and above, are overweight. The federation projects that 4 billion people – half of the global population over the age of five – are likely to be overweight or obese by 2035.
What is particularly alarming is the swift rise in obesity rates in lower-income countries. Among the ten countries projected to experience the most significant surges in obesity, nine belong to the low or lower-middle-income countries. All of these countries are located in Asia or Africa.
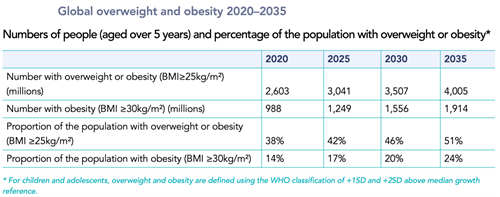
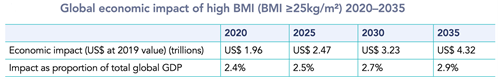
The report further quantifies that the annual cost of humanity’s growing obesity problem will reach $4 trillion in 2035, or 2.9% of global GDP, assuming no improvements in prevention and treatment measures. These costs arise both from increased spending on health care and from lost working time due to illness and premature deaths. This financial toll is equivalent to experiencing another COVID-19 pandemic every year, considering that the virus caused the world economy to shrink by 3% of GDP during 2020, the pandemic’s worst year (World Bank, 2022).
This increased prevalence of obesity across age, sex, and ethnic groups points to a complex network of biological, psychological, and local environmental factors - often difficult to measure - that influence obesity. This inherent complexity is frequently overlooked in favor of viewing overweight and obesity as mere issues of willpower, thus hindering regulatory action and emphasizing personal responsibility. However, it seems very unlikely that a sudden and simultaneous decline in willpower could explain the current and projected figures. Whether labelled a disease or not, tackling obesity will require a broad, coordinated effort.
Prevention Or Treatment?
To rein in the obesity epidemic, two important policy pillars must be considered: prevention and treatment.
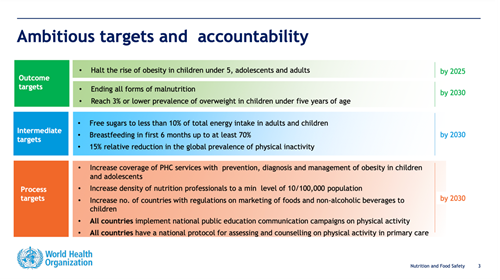
On the prevention front, (inter)governmental organizations, spearheaded by the WHO, continue to focus on preemptive measures. During the 75th World Health Assembly in 2022, Member States adopted new recommendations for both the prevention and management of obesity and endorsed the WHO Acceleration Plan to Stop Obesity. The plan focuses on 5 workstreams:
- Funding/Building Capacity: This includes a proposal for implementing an additional 20% tax on sugar-sweetened beverages to deter consumption.
- Showcases of Frontrunner Countries: Highlighting success stories from nations leading the fight against obesity, such as Portugal, Slovenia and the UK.
- Increasing Awareness: Utilizing media and scientific papers to spread knowledge and understanding of obesity's risks and prevention methods.
- Connecting Stakeholders: Encouraging collaboration among various entities, including other UN agencies and the private sector, to foster a united front against obesity.
- Installing Monitoring: Establishing comprehensive delivery plans to track and assess the implementation and success of the anti-obesity measures.
The plan sets out clear targets by 2030:
In contrast to prevention efforts, the treatment front has seen the emergence of a new generation of GLP1 medicines in the fight against obesity. Inspired by celebrities’ body transformations, Novo Nordisk has benefited greatly from a surge in demand from patients for its semaglutide medicine — branded as Ozempic for diabetes and Wegovy for weight loss. Even to the extent that the success in the US influences the economy of Denmark (USD sales have to be converted into DKK – see WSJ article). Competitor Eli Lilly awaits approval for a similar drug, Tirzepatide, with promising testing results. Their Mounjaro drug, a diabetes medicine with the same active ingredient, is already available on the market.
With physicians prescribing GLP1s like Wegovy, claiming health benefits beyond mere weight reduction – such as improvement in patients’ blood pressure and cholesterol – expectations only increased. To obtain proof, Novo Nordisk invested in its largest-ever trial, tracking over 17,000 people since 2018. Preliminary results, published last week, revealed that Wegovy reduces the risk of heart attacks and strokes by 20%. However, Novo Nordisk has only shared the topline results from the trial, leaving practitioners waiting for the details to draw meaningful conclusions.
Still, the results from Novo’s study are a major shift from older weight loss drugs that were found to cause heart problems. For example, in the late 1990s, the two drugs that made up fen-phen, once a hugely popular weight loss combination, were pulled from the market after they were linked to heart valve problems.
In any case, these test results, the further expansion of the obesity pandemic and now also the first launches of Wegovy in Europe (Germany) have further sharpened the debate around the treatment of obesity and possible reimbursements. While private insurers in the United States will cover GLP1 drugs for people with diabetes, they have been slower to pay for their use in people with obesity. A 2022 survey found that just 22% of employers in the US pay for weight-loss medicines. Some 45%, meanwhile, cover bariatric surgery, for which the longer-term health benefits are well established. And several media reports suggest that some employers that initially agreed to cover Wegovy are reversing course, while others are greatly narrowing the criteria for eligibility. Their concerns over costs, at a list price of about $1,300 a month, are valid. The drugs, which must be taken continuously in order to keep the pounds off, are expensive. Meanwhile, those employers fear they won’t be the beneficiaries of long-term savings if people move on to another job. At the same time US Congress has yet to open the door for Medicare (US federal health insurance for people 65 or older) to pay for any obesity medicines. In Europe public health systems are restricting who qualifies for it. The UK’s National Institute for Health and Care Excellence (Nice), for example, will pay for it for patients at the higher end of the body mass index, who already have at least one weight-related condition, and then for only two years (despite evidence showing that if you stop taking the drug, you regain weight). Also, in this case the fear is that the large percentage of people on (public) insurance who would qualify for the drugs would be budget-busting.
True Costs and Benefits
While some individuals resist labeling obesity as a disease, dismissing weight loss drugs as mere vanity products, recent study results provide at least some support treating obesity as a legitimate medical condition. One thing that would help the overall discussion about access to medicines as a complement to prevention is a better accounting of the potential costs and savings of these drugs.
The World Obesity Federation has made an attempt to estimate the economic cost of obesity, but these figures fluctuate widely depending on the methods of calculation. A careful analysis, grounded in emerging clinical and real-world data, could foster more honest conversations about the value of these medicines to society. It could also assist in weighting the immediate costs against the long-term benefits.
The burden of obesity and obesity-related conditions is unquestionably high, but the value of insurance coverage of anti-obesity medications unfortunately today remains unclear. A more nuanced understanding of the economic implications could help bridge this gap and provide a clearer perspective on the role of medications in combating obesity.
