Stijn Plessers holds a degree in Economics (Catholic University of Leuven). He started his career in 2006 at a private bank and then worked for KBC Asset Management for 15 years. At KBC AM, he was originally responsible for managing a large credit and OTC derivatives portfolio before focusing entirely on equities. First as an analyst for the technology sector and then as a manager of specialized, global equity mandates. In April 2023, Stijn made the switch to Econopolis Wealth Management.
Biden and trump seemingly align on U.S. Healthcare policies! Do they?

No matter how vast their differences may be, both presidential candidates will share at least one common stance in the lead-up to the elections. Like almost every presidential candidate in the (recent) past, they will be outspoken in their criticism of the American healthcare system. This critique remains a consistent theme, whether they are campaigning for or occupying the Oval Office, even though tangible changes often seem elusive.
“On too many nights, too many Americans lay in bed staring at the ceiling, worrying what will happen if their spouse gets sick, if their child gets sick, or if something else happens to them.” Joe Biden – 29/08/2023
“The best thing that is happening with the health care is premiums will come down. … We're going to have a tremendous - tremendously competitive market and health care costs are going to be forced down.” Donald Trump – 02/05/2017
Both statements highlight the widespread concern over the existing healthcare system. Despite no country investing as much per capita in healthcare, improvements in life expectancy in the U.S. do not appear to correlate accordingly. Just this week, Politico - a prominent political journalism organization - disclosed the White House's intention to unveil a new 'task force' aimed at tackling the escalating costs of healthcare.
Comparison of life expectancy and health expenditure in 2021
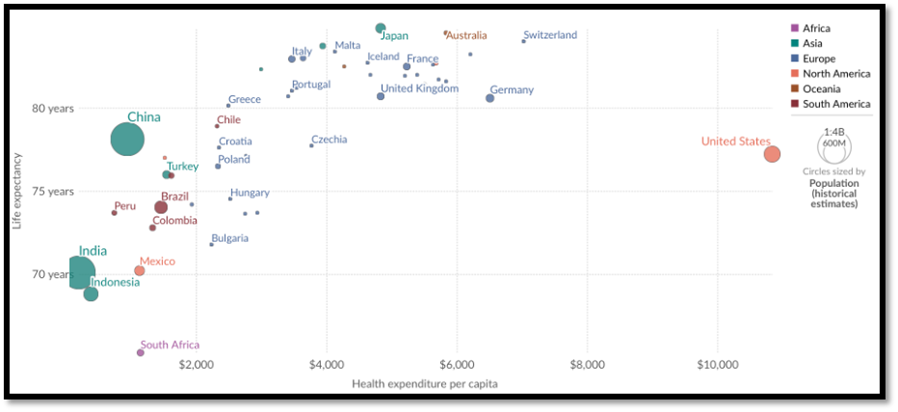
Source: Our World in Data (https://ourworldindata.org/grapher/life-expectancy-vs-health-expenditure)
Brief history of U.S. Healthcare
We attempt to provide a brief history to understand the current system and its challenges. The United States healthcare system is a complex patchwork consisting of private insurers, public programs, hospitals, physicians, and various other providers. Unlike many other developed nations, the U.S. does not have a universal healthcare system, leaving millions of Americans without adequate medical coverage.
The roots of the current system can be traced back to the 19th century when the rise of medical professionalism occurred, followed by the establishment of the American Medical Association (AMA), and the beginnings of employer-sponsored health insurance. The early 20th century witnessed significant scientific advancements, transforming medicine from a largely anecdotal practice to a science-based discipline. Hospitals became centers of care, and medical costs began their steady ascent. During the Great Depression and World War II, proposals for national health insurance surfaced but failed to gain traction due to fierce opposition from the AMA and concerns about "socialized medicine".
In the aftermath of World War II, private health insurance expanded, predominantly tied to employment. The enactment of Medicare and Medicaid in 1965 was pivotal, offering public health coverage to the elderly and the poor. Despite these advancements, a considerable number of Americans remained without insurance coverage.
U.S. Healthcare: private over public
Today, the U.S. healthcare system remains a mixed model (both private & public) with these key components:
- Employer-Based Insurance: The dominant source of health insurance, covering over half of the non-elderly population. However, rising premiums and deductibles have strained this model.
- Medicare: A federal program providing health insurance for Americans aged 65 and older and those with certain disabilities.
- Medicaid: A joint federal-state program offering health coverage to low-income individuals and families.
- Individual Marketplaces: Established under the Affordable Care Act (ACA, also known as Obamacare), these marketplaces allow individuals to purchase private insurance, often with government subsidies.
- Other: Other: Veterans Health Administration (VA), Children's Health Insurance Program (CHIP), and Indian Health Service (IHS) provide additional coverage for specific populations.
Despite significant strides in medical technology and access to care, the U.S. healthcare system faces several deeply entrenched challenges. As illustrated earlier, the U.S. spends far more on healthcare per capita than any other developed nation, yet health outcomes often lag behind. Administrative complexity, expensive pharmaceuticals, and a lack of price transparency contribute to skyrocketing healthcare costs. Medical debt is a crushing burden for many Americans. In addition to affordability, access also remains problematic for part of the population. Health insurance coverage remains a major determinant of access to care. The uninsured and underinsured face significant barriers to necessary medical services.
The current system yields inconsistent outcomes. The prevalence of fee-for-service payment models may prioritize volume rather than quality of care, and the system's fragmented nature can result in inefficiencies and discontinuities in care coordination. Additionally, the scarcity of primary care physicians in many U.S. regions affects preventive care and chronic condition management. This shortfall is exacerbated by an emphasis on specialized medicine and the high costs associated with medical education.
All of this takes place against the background of a devastating opioid epidemic and a broader mental health crisis. Access to quality addiction treatment and mental health services is often inadequate, leaving many struggling.
Endless debate (club)
The challenges facing the U.S. healthcare system are substantial and have always sparked intense political debates. Broadly speaking, potential solutions fall into four different categories. Some suggest incremental reforms by focusing on expanding coverage options like Medicaid, strengthening the ACA, and regulating prescription drug prices. Others advocate a more market-based approaches like promoting price transparency, greater competition among insurers, and consumer-driven healthcare. More radical voices want to replace the fragmented private insurance system with a government-run healthcare plan ("Medicare for All") that guarantees universal coverage. Finally, there are proposals for possible combinations of public and private insurance, such as a public option within healthcare marketplaces.
Besides the complex interplay of cost, access and quality, other important considerations should be included in the debate. Harnessing the potential of rapid technological innovation, like health information technology, telehealth, and artificial intelligence can drastically affect outcomes. Focusing on prevention by investing in preventive health measures (and addressing social determinants of health) should improve overall population health and reduce long-term costs. Finally, empowering patients by encouraging involvement in decision-making and promoting health literacy could foster informed choices and better health outcomes.
While the challenges are significant, the American system is not without benefits. In mostly public systems, the healthcare ecosystem is more streamlined, with the government playing a central role. This allows the government to maintain lower prices, but this does not incentivize innovation. Healthcare providers (the government) don’t need to earn a financial return, so prices and costs can stay lower. Healthcare providers (the government) lack an incentive to innovate since there is little to no (immediate) financial reward. In the U.S. on the other hand healthcare providers directly benefit from the financial rewards of innovation, incentivizing progress.
Can U.S. Healthcare change?
The history of U.S. healthcare is a story of both progress and persistent shortcomings. The current system offers advanced medical treatments and a high degree of choice for some, but also leaves many behind due to costs and access barriers. The debate over how to provide affordable and high-quality healthcare for all Americans will undoubtedly continue this election year. However, there is once again a good chance that the rhetoric will not result in reforms of this deeply entrenched system.
